Organ systems work together with other organ systems to keep the body in good health - Human Body Systems.
An organ system is a group of organs that work together in the body to perform a complex function, such as pumping blood or processing and utilizing nutrients. There are 11 major organ systems in the human body:
🔵The circulatory system
🔵The lymphatic system
🔵The respiratory system
🔵The integumentary system
🔵The endocrine system
🔵The gastrointestinal (digestive) system
🔵The urinary (excretory) system
🔵The musculoskeletal system
🔵The nervous system
🔵The reproductive system
🔵The immune system
Organ systems work together with other organ systems to keep the body in good health. For example, the circulatory and digestive systems work together to deliver nutrients throughout the body. With the exception of the reproductive system, each is necessary for survival.
Circulatory System
The circulatory system transports oxygen and nutrients to all corners of the body. It also carries away carbon dioxide and other waste products.
The blood circulatory system, also called the cardiovascular system, consists of the heart and the blood vessels that run throughout the body. It delivers nutrients and oxygen to all cells of the body.
The oxygen we breathe gets mixed into the blood in the lungs, and the heart pumps this blood to all parts of the body. Each heartbeat is a contraction of the heart as it pumps blood around the body.
The heart has four chambers: the left atrium, right atrium, right ventricle and left ventricle. They are all separated by one-way valves, meaning the blood can only flow in one direction. Blood is carried to the heart in the veins, and back out to the rest of the body in the arteries.
the cardiovascular system at large, which includes the:
Heart
Blood vessels (arteries and veins)
The blood itself
In order for blood to make it everywhere it needs to go, the circulatory system maintains the blood flow within a certain pressure range.
Blood pressure that’s too high puts extra stress on other organs and tissues. Low blood pressure means the blood—and its nutrients—won’t make it to where it needs to go.
diseases that affect the circulatory system, as well as treatment options and prevention.
Fifteen circulatory system disease The cardiovascular system is composed of the heart and blood vessels.
Diseases that can affect the circulatory system include:
1. Atherosclerosis
Atherosclerosis is a hardening of the arteries.
It is typically caused by a diet high in fat, which leaves fatty deposits on the lining of the blood vessels. These fatty deposits stick together and make the arteries hard and less flexible.
Atherosclerosis leads to high blood pressure, which can damage the heart and kidneys and even lead to strokes.
2. Heart attack
Myocardial infarction (MI) is the technical term for a heart attack. A heart attack can occur when the blood supply is cut off from the heart, often by a blood clot. Some heart attacks are minor, but others can be life-threatening.
3. Mitral valve prolapse
Mitral valve prolapse means the mitral valve bulges out or prolapses because it does not close evenly. The mitral valve pumps freshly oxygenated blood out of the heart to the rest of the body.
4. Mitral valve regurgitation
Mitral valve regurgitation happens when the mitral valve does not close all the way and causes a leak, allowing some of the oxygenated blood to flow backward.
5. Mitral stenosis
Mitral stenosis means the mitral valve is abnormally narrow which can prevent the blood from flowing smoothly or quickly through it.
6. Angina pectoris
Angina pectoris means “pain in the chest” and occurs if the heart is not receiving enough blood. People often describe it as a crushing sensation or feeling like their chest is in a vice.
People with angina pectoris may also feel breathless, tired, and nauseated.
7. Arrhythmia and dysrhythmia
Arrhythmia and dysrhythmia are often used interchangeably, and both refer to abnormal heart rates and rhythms. In general, arrhythmia means “no rhythm” and dysrhythmia means “abnormal rhythm.”
8. Cardiac Ischemia
Cardiac ischemia may cause similar pain to a heart attack. Cardiac ischemia means the heart muscle is not getting enough oxygen to function properly. A person with cardiac ischemia will usually experience angina-like pain and may feel as though they are having a heart attack.
9. High cholesterol
High cholesterol is usually caused by a sedentary lifestyle and an unhealthful diet. Some people can also be genetically at risk of high cholesterol.
People need cholesterol, but too much cholesterol can form a thick layer on the inside of the vessels, blocking blood flow.
10. Heart failure
Heart failure means that the heart is not pumping blood around the body as efficiently as it should. It can lead to fatigue, shortness of breath, and coughing.
Some people with heart failure find it difficult to do things such as walking, climbing stairs, or carrying groceries.
11. High blood pressure (hypertension)
High blood pressure or hypertension means the force or pressure of the blood flowing through the vessels is consistently too high. High blood pressure can lead to stroke, loss of vision, heart failure, heart attack, kidney disease, and reduced sexual function.
12. Stroke
A stroke can happen when one of the vessels that lead to the brain either becomes blocked by a blood clot or bursts. This stops blood flow and prevents oxygen from getting to the brain.
13. Peripheral artery disease (PAD)
Peripheral artery disease (PAD) refers to narrowing of the arteries that lead to the legs, stomach, arms, and head. This reduced blood flow can damage the cells and tissues in the limbs, organs, and brain. PAD tends to occur more often in older people.
14. Venous thromboembolism (VTE)
Venous thromboembolism (VTE) is a blood clot that gets stuck in a vein, blocking the flow of blood. It is a serious condition that needs emergency medical attention.
15. Aortic aneurysms
Aortic aneurysms affect the main artery in the body. It means the artery wall has weakened, allowing it to widen or “balloon out.” An enlarged artery could burst and become a medical emergency.
How can I prevent disease of the circulatory system?
One of the most important ways to prevent circulatory system diseases is to visit your healthcare provider for annual checkups. Many people have risk factors they don’t even know about. Your provider can catch problems early before they become more serious.
Dietary changes and lifestyle changes can also help you prevent circulatory system diseases. These include:
🔵Follow a heart-healthy diet.
🔵Build aerobic exercise into your daily routine.
🔵Avoid smoking, tobacco use and street drugs.
Talk with your provider about changes that are healthy for you. Be sure to check with them before starting any new exercise plan.
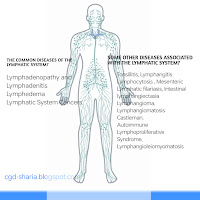
Lymphatic System
How Your Circulatory System Works Lymphatic System.The lymphatic system is the drainage system of the body. It plays an important role in your immunity, blood pressure regulation, digestion, and other functions.
WHAT IS THE LYMPHATIC SYSTEM?
The lymphatic system consists of lymph nodes, lymphatic vessels, and lymphatic organs. These lymphatic system components are involved in moving lymphatic fluid or lymph into the bloodstream.
Lymph is a clear, watery fluid. It is the fluid that remains in the body tissues after the arteries, arterioles, and blood capillaries have delivered nutrient-rich blood, and the veins have removed nutrient-poor blood and waste material from tissues throughout the body. The lymphatic system rounds up the excess fluid (lymph) from the body’s tissues, processes it, and ultimately delivers it back to the bloodstream.
WHAT ARE THE COMPONENTS OF THE LYMPHATIC SYSTEM?
The lymphatic system has many parts, including:
Lymph or lymphatic fluid
Lymph is the excess fluid that drains from tissues. It contains substances such as fats, proteins, minerals, nutrients, cancer cells, foreign organisms like bacteria and viruses, white blood cells, and other immune system cells.
Lymph Nodes
These are small glands that look like kidney beans. They filter and clean the lymphatic fluid when it passes through them. Lymph nodes also make and store cells of the immune system to fight harmful substances found in the lymph. There are more than 500 lymph nodes distributed throughout the body. They can occur as a solitary lymph node or as a chain of lymph nodes. The neck, armpits, and groin are common locations for regional lymph nodes.
Lymphatic Vessels or Lymphatic Ducts
These are interconnected capillaries (tiny blood vessels or small lymphatic vessels) that carry lymph from the tissues to the lymph nodes and ultimately into large lymphatic vessels known as the collecting ducts. Lymphatic vessels work much like veins and have valves to keep the lymphatic flow moving towards the collecting ducts. There are two collecting ducts in the body, the left and right lymphatic duct (the left lymphatic duct is also called the thoracic duct). The collecting ducts return the lymph to the blood circulation by emptying into the venous circulation, specifically the subclavian veins under the collarbone.
Spleen, Thymus, Tonsils and Adenoids, Bone Marrow, Peyer’s Patches, and Appendix.
These lymphatic organs or lymphoid tissue filter lymph, produce and store immune system cells, and fight off foreign organisms and infections. The spleen is the largest lymphatic organ in the body.
WHY IS THE LYMPHATIC SYSTEM IMPORTANT?
The lymphatic system plays many important functions in the body, such as:
Maintains fluid balance by collecting excess fluid from tissues all over the body and taking it back to the bloodstream. Returning lymph to the circulation helps to maintain normal blood volume and blood pressure and prevents edema (the buildup of excess fluid in the tissues).
Absorbs fats and proteins from the digestive tract and carries it back to the circulatory system through the lymph fluid.
Produces lymphocytes (white blood cells) and other immune cells to fight infection and protect against foreign particles like bacteria and viruses (the lymphatic system is a part of the body’s immune system).
Removes abnormal cells and waste products from the lymph fluid.
WHAT ARE THE COMMON DISEASES OF THE LYMPHATIC SYSTEM?
There are several conditions that can affect the lymph vessels, lymph nodes, and lymphatic organs. The three most common lymphatic diseases include:
Lymphadenopathy and Lymphadenitis
Lymphadenopathy is the medical term for swollen or enlarged lymph nodes. It can occur due to inflammation, infection, or cancer. When the cause of a swollen lymph node is infections or inflammatory disorders, it is called lymphadenitis. For example, strep throat can cause enlargement of regional lymph nodes in the neck. Breast cancer can lead to enlarged lymph nodes in the axillae (armpits).
Lymphedema
This medical term refers to a buildup of lymphatic fluid in the tissues. It most commonly occurs in the arms and legs. Lymphatic system blockages can cause lymphedema due to scar tissue, tumors, or damaged lymph nodes or lymph vessels. Lymphedema can also occur when lymph nodes are surgically removed or subjected to radiation during cancer treatment. Severe lymphedema can be painful, disabling, and disfiguring and can put a person at risk of serious infections.
Lymphatic System Cancers
When lymphocytes (white blood cells) multiply uncontrolled, it can result in a cancer called lymphoma. Two common types of lymphoma are Hodgkin lymphoma and non-Hodgkin lymphoma.
WHAT ARE SOME OTHER DISEASES ASSOCIATED WITH THE LYMPHATIC SYSTEM?
Some other disorders that can affect the body’s lymphatic system include:
Tonsillitis: An infection and inflammation of the tonsils in the throat.
Lymphangitis: An inflammation of the lymphatic vessels.
Lymphocytosis: The presence of too many white blood cells.
Mesenteric lymphadenitis: An inflammation of lymph nodes in the mesentery (an organ attached to the intestines in the abdomen).
Lymphatic filariasis: A parasitic infection of the lymphatic system that leads to massive swelling in the arms, legs, and genitals.
Intestinal lymphangiectasia: A condition in which lymph is lost in the small intestine, leading to protein loss.
Lymphangioma: A congenital disorder (present from birth) in which there is a malformation of the lymphatic system.
Lymphangiomatosis: A condition characterized by the occurrence of widespread lymphatic vascular malformations.
Castleman Disease: A condition in which there is an overgrowth of lymphatic system cells.
Autoimmune Lymphoproliferative Syndrome: A rare genetic condition associated with an excessive number of white blood cells in the lymph nodes, spleen, and liver.
Lymphangioleiomyomatosis: A rare disorder in which abnormal cells resembling muscle cells grow uncontrolled in the lymph nodes, kidneys, and lungs.
How can I keep my lymphatic system healthy?
To keep your lymphatic system strong and healthy, you should:
Avoid exposure to toxic chemicals like those in pesticides or cleaning products. These chemicals can build up in your system and make it harder for your body to filter waste.
Drink plenty of water to stay hydrated so lymph can easily move throughout your body.
Keep a healthy lifestyle that includes regular exercise and
a nutritious diet. Your provider can give you specific advice tailored to your
medical history and needs.
Restoring and enhancing the flow of your lymphatic system
can help the following conditions:
Injuries, post-surgical scar tissue/swelling
Pain and InflammationKeep a healthy lifestyle that includes
regular exercise and a nutritious diet. Your provider can give you specific
advice tailored to your medical history and needs.
Restoring and enhancing the flow of your lymphatic system
can help the following conditions:
- Injuries,
post-surgical scar tissue/swelling
- Pain
and Inflammation
- Edema,
Lymphedema
- Breast
conditions/fibrosis
- Sinus
conditions and allergies
- Recovery
post esthetics procedures
- Skin
Aging
- Scars
- Acne
- Digestive
Issues
- Stress
Benefits of Lymphatic Drainage
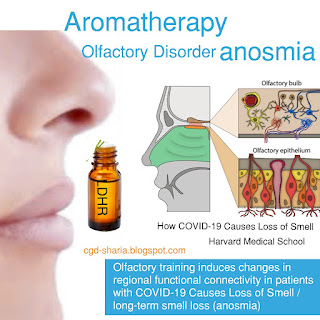
Respiratory System
The respiratory system is responsible for breathing, which is the controlled movement of air in and out of the body (ventilation). It also moves oxygen and carbon dioxide into and out of the bloodstream (respiration).
This organ system contains the:
Lungs
Trachea (windpipe)
Airways of the respiratory tree
One of the least understood responsibilities of the respiratory system is to help regulate the body’s pH balance, or the body’s balance of acids and bases.
Carbon dioxide is made into carbonic acid, which affects the pH balance. The respiratory system regulates this pH level when it releases carbon dioxide from the body.3 Breathing issues may indicate a condition that affects the body’s acidity.
What Is the Respiratory System?
The respiratory system is the organs and other parts of your body involved in breathing, when you exchange oxygen and carbon dioxide.
Parts of the Respiratory System
Your respiratory system includes your:
Nose and nasal cavity
Sinuses
Mouth
Throat (pharynx)
Voice box (larynx)
Windpipe (trachea)
Diaphragm
Lungs
Bronchial tubes/bronchi
Bronchioles
Air sacs (alveoli)
Capillaries
Respiratory System Diseases
Common diseases of the respiratory system include:
Asthma. Your airways narrow and make too much mucus
Bronchiectasis. Inflammation and infection make your bronchial walls thicker.
Chronic obstructive pulmonary disease (COPD). This long-term condition gets worse over time. It includes bronchitis and emphysema.
Pneumonia. An infection causes inflammation in your alveoli. They might fill up with fluid or pus.
Tuberculosis. A bacterium causes this dangerous infection. It usually affects your lungs but might also involve your kidney, spine, or brain.
Lung cancer. Cells in your lung change and grow into a tumor. This often happens because of smoking or other chemicals you’ve breathed in.
Cystic fibrosis. This disease is caused by a problem in your genes and gets worse over time. It causes lung infections that don’t go away.
Pleural effusion. Too much fluid builds up between the tissues that line your lungs and chest.
Idiopathic pulmonary fibrosis. Your lung tissue becomes scarred and can’t work the way it should.
Sarcoidosis. Tiny clumps of inflammatory cells called granulomas form, often in your lungs and lymph nodes.
Additional Illness – COVID-19
Preventative Measures for Respiratory Disease
number one piece of advice to avoid respiratory system illnesses is to stop smoking and preferably, never start.
practice avoidance in order to prevent respiratory disease. That includes avoiding sick people and places with a lot of dust or harsh chemicals.
focus on the basics, too. Try to maintain a healthy weight, get adequate sleep, decrease stress, add plenty of activity and eat a balanced diet.
An Overview of Respiratory Failure
Integumentary System
The integumentary system is unique because it is the largest and only single-organ system in the body. It protects the body from the external environment and helps regulate body temperature.
Sweat glands
Hair follicles
Nails
Nerves
What are skin diseases?
Your skin is the large organ that covers and protects your body. Your skin has many functions. It works to:
Hold in fluid and prevent dehydration.
Help you feel sensations, such as temperature or pain.
Keep out bacteria, viruses and other causes of infection.
Stabilize your body temperature.
Synthesize (create) vitamin D in response to sun exposure.
Skin diseases include all conditions that clog, irritate or inflame your skin. Often, skin diseases cause rashes or other changes in your skin’s appearance.
What are the most common types of skin diseases?
Some skin diseases are minor. Others cause severe symptoms. Some of the most common skin diseases include:
Acne, blocked skin follicles that lead to oil, bacteria and dead skin buildup in your pores.
Alopecia areata, losing your hair in small patches.
Atopic dermatitis (eczema), dry, itchy skin that leads to swelling, cracking or scaliness.
Psoriasis, scaly skin that may swell or feel hot.
Raynaud’s phenomenon, periodic reduced blood flow to your fingers, toes or other body parts, causing numbness or skin color change.
Rosacea, flushed, thick skin and pimples, usually on the face.
Skin cancer, uncontrolled growth of abnormal skin cells.
Vitiligo, patches of skin that lose pigment.
What are some types of rare skin diseases?
Many rare skin diseases are genetic, meaning you inherit them. Some rare skin diseases include:
Actinic prurigo (AP), itchy rash in response to sun exposure.
Argyria, changes in skin color due to silver buildup in your body.
Chromhidrosis, colored sweat.
Epidermolysis bullosa, a connective tissue disorder that causes fragile skin that blisters and tears easily.
Harlequin ichthyosis, thick, hard patches or plates on the skin that are present at birth.
Lamellar ichthyosis, waxy skin layer that sheds in the first few weeks of life, revealing scaly, red skin.
Necrobiosis lipoidica, rash on the lower legs that can develop into ulcers (sores).
How can I prevent skin diseases?
Some skin diseases are not preventable. For example, there is no way to change your genetics or prevent an autoimmune disorder.
You can take steps to avoid contagious or infectious skin diseases. You may prevent contagious skin diseases or reduce their symptoms if you:
Avoid sharing utensils, personal items or cosmetics.
Disinfect objects you use in public spaces, such as gym equipment.
Drink plenty of water and eat a nutritious diet.
Limit contact with irritants or harsh chemicals.
Sleep seven to eight hours per night.
Use sun protection to prevent sunburn and other sun damage.
Wash your hands regularly with soap and water.
The Skin and How It Works
Endocrine System
The endocrine system mostly regulates metabolism and uses the products of digestion. Along with the nervous system and immune system, it’s generally considered one of the most complicated systems in the body.
This organ system includes all the glands that secrete hormones into the bloodstream, including:
Adrenal
Gonads (ovaries and testicles)
Hypothalamus
Pancreas
Parathyroid
Pineal
Pituitary
Thymus
Thyroid
Endocrine System
The endocrine system consists of 8 glands that produce hormones. Hormones act as chemical messengers that travel through the bloodstream to your tissues and organs.
They influence all your body processes and are responsible for reproduction, growth and development, metabolism, sexual function, and your mood.
There are two major types of Endocrine disorders. These include
Endocrine disease due to a hormonal imbalance
Endocrine disease due to formation of lesions in the endocrine system
Let’s take a look at some of the endocrine disorders that occur due to hormonal imbalance.
Diabetes
Diabetes is the most common type of endocrine disorder. Type I diabetes is an autoimmune disease where your pancreas stops producing the hormone insulin. As a result, your body is unable to maintain an appropriate amount of blood sugar levels in the bloodstream. Type II diabetes occurs when your body develops insulin resistance. As a result, it cannot use insulin properly.
Addison’s Disease
Addison’s disease is an endocrine disorder that develops when your adrenal glands do not release sufficient amounts of the hormone cortisol. This is referred to as adrenal insufficiency. Adrenal insufficiency can result when there is a problem in the adrenal glands. It can also be due to problems in the transfer of information from the brain to the adrenal glands, instructing them to produce cortisol. In some cases, adrenal insufficiency also involves low production of the hormone aldosterone.
Gigantism
Gigantism, also known as acromegaly, is a type of growth hormone disorder. It occurs when the pituitary gland produces excessive amounts of somatotropin (the growth hormone). As a result of this endocrine disorder, a child’s body parts and their bones grow abnormally fast. Their girth as also affected.
Polycystic Ovary Syndrome
Polycystic ovary syndrome (PCOS) is a hormonal disorder that occurs in women between the ages of 18 to 44. It interferes with the development and release of eggs from your ovaries. The ovaries can develop numerous follicles as well. PCOS is a leading cause of infertility in women. The exact cause of this syndrome is not known. Some common factors that can lead to PCOS include:
Excess production of insulin.
Heredity factors.
The overproduction of the hormone androgen by the ovaries.
Let’s Sum It Up.
TYPES OF ENDOCRINE DISORDERS
Endocrinology is the branch of medicine that focuses on endocrine glands and hormones in the body. Hormones regulate many bodily functions; however, when a hormone imbalance occurs, it can have a variety of effects on the body. The Diabetes Center & Endocrinology Clinic at UI Health offers comprehensive services and treatments for patients that suffer from hormonal imbalances and endocrine disorders,. We provide treatment options for many types of metabolic and endocrine disorders, including:
Adrenal Insufficiency
Adrenal glands, located on top of the kidneys, produce various hormones. Adrenal insufficiency occurs when the adrenal glands do not produce sufficient amounts of steroid hormones — primarily cortisol, which regulates sodium conservation, potassium secretion, and water retention.
Congenital Adrenal Hyperplasia (CAH)
Congenital adrenal hyperplasia (CAH) is a group of inherited genetic disorders that affect the adrenal glands. A person with CAH lacks one of the enzymes the adrenal glands use to produce hormones that help regulate metabolism, the immune system, blood pressure, and other essential functions.
Hyperaldosteronism
Hyperaldosteronism is a disease where the adrenal glands make too much aldosterone, a hormone that stimulates absorption of sodium by the kidneys and helps to regulate water and salt balance in the body. When too much aldosterone is produced, this leads to hypertension (high blood pressure) and low blood potassium levels.
Osteoporosis
Osteoporosis is the deterioration of bone tissue and reduction of bone strength, making bones fragile. Osteoporosis makes the wrist, hip, spine and other parts of the skeleton vulnerable to fractures. Falls in people with osteoporosis can lead to serious health consequences.
Pituitary Disorders
Pituitary tumors are abnormal growths that develop in your pituitary gland. Some pituitary tumors result in too many of the hormones that regulate important functions of the body; others can cause the pituitary gland to produce lower levels of hormones. Most pituitary tumors are noncancerous (benign) growths (adenomas). Adenomas remain in your pituitary gland or surrounding tissues and don't spread to other parts of your body.
Thyroid Disorders
The thyroid gland is an endocrine gland that is located in the front of the neck. This gland produces thyroid hormones that primarily influence the body's metabolism and protein synthesis. Abnormal cell growth in the thyroid gland can lead to thyroid cancer. The thyroid also can be affected by a variety of diseases, including:
Hypothyroidism: Hypothyroidism is an underactive thyroid gland, and the thyroid gland can't make enough thyroid hormone to keep the body running normally. Individuals are hypothyroid if they have too little thyroid hormone in the blood. Common causes are autoimmune disease, surgical removal of the thyroid, and radiation treatment.
Hyperthyroidism: Hyperthyroidism is a condition in which the thyroid gland is overactive and makes excessive amounts of thyroid hormone. When the thyroid gland is overactive, the body's processes speed up, and individuals may experience nervousness, anxiety, rapid heartbeat, hand tremors, excessive sweating, weight loss, and sleep problems, among other symptoms.
A healthy endocrine system The endocrine system is influenced by factors in your health, lifestyle choices, and your daily stress levels which must all be addressed to keep it healthy.
How to keep endocrine system healthy :
You can take care of your endocrine system by engaging in a healthy and active lifestyle.
There are several things that can be done to keep the endocrine system healthy including eating a healthy diet and avoiding sugar,
alcohol, preservatives, and unhealthy fats. Calcium and vitamins B, C, and D are also important as are Omega 3, 6 and 9 fatty acid oils. Additional measures include drinking plenty of water, getting plenty of rest, practicing stress reduction techniques, and exercising.
There are many different kinds of endocrine disorders. They usually result due to hormone imbalance. Most endocrine disorders can be treated if they are diagnosed early. The symptoms of these disorders can vary from person to person. They also depend on the gland involved.
Use Lavender Dreamyy DETOXIFICATION improved endocrine system and be blanched.
The Endocrine System and How It Work
Gastrointestinal (Digestive) System
The gastrointestinal (GI) system is sometimes referred to as the gut or the digestive system. It is responsible for breaking down foods into nutrients, which the body needs for energy, growth, and cell repair. This system includes all the organs that carry food from where it enters the body to where it exits, including the:
Mouth
Esophagus
Stomach
Small intestine
Large intestine
Rectum
Anus
The pancreas, gallbladder, and liver are also part of this organ system.
The GI tract and the endocrine system have a lot of interaction. The endocrine system produces the hormones that regulate digestion and the absorption of nutrients.
The GI system also owes a lot to the vagus nerve, the main contributor to the parasympathetic nervous system, which regulates bodily functions. The vagus nerve is involved in slowing metabolism, lowering heart rate and blood pressure, and stimulating the mechanics of digestion.
How Your Digestive System Works
One Organ, Two Organ Systems
Some organs belong to more than one organ system. The pancreas, for example, can be considered a part of the digestive system because it secretes enzymes that help the body break down fat, protein, and starch. It is also part of the endocrine system because it produces hormones that help regulate blood sugar.
What are functional gastrointestinal diseases?
Functional diseases are those in which the GI tract looks normal when examined, but doesn't move properly. They are the most common problems affecting the GI tract (including your colon and rectum). Constipation, irritable bowel syndrome (IBS), nausea, gas, bloating and diarrhea are common examples.
What are some of the common gastrointestinal diseases that healthcare providers treat?
Some of the most common conditions they treat include:
Constipation
Constipation, which is a functional problem, makes it hard for you to have a bowel movement (or pass stools), the stools are infrequent (less than three times a week), or incomplete. Constipation is often related to inadequate "roughage" or fiber in your diet, or a disruption of your regular routine or diet.
Constipation causes you to strain during a bowel movement. It may cause small, hard stools and sometimes anal problems such as fissures or hemorrhoids. Constipation is rarely the sign that you have a more serious medical condition.
You can treat your constipation at home by:
Increasing the amount of fiber and water to your diet
Exercising regularly and increasing the intensity of your exercises as tolerated.
Moving your bowels when you have the urge (resisting the urge causes constipation).
If these treatment methods don't work, laxatives can be useful. Always follow the instructions on your laxative medicine, as well as the advice of your healthcare provider.
Irritable bowel syndrome (IBS)
Irritable bowel syndrome (also called spastic colon, irritable colon, IBS, or nervous stomach) is a functional condition where your intestinal muscles contract more or less often than “normal.” Certain foods, medicines and emotional stress are some factors that can trigger IBS.
Symptoms of IBS include:
Abdominal pain and cramps.
Excess gas.
Bloating.
Change in bowel habits such as harder, looser, or more urgent stools than normal.
Constipation and/or diarrhea.
You can treat IBS at home by:
Avoiding excessive caffeine.
Increasing fiber in your diet.
Monitoring which foods trigger your IBS (and avoiding these foods).
Minimizing stress or learning different ways to cope with stress.
Taking medicines as prescribed by your healthcare provider.
Avoiding dehydration, and hydrating well throughout the day.
Getting high quality rest/sleep.
Hemorrhoids
Hemorrhoids are dilated veins in your anal canal. This is a structural disease. They're caused by chronic excess pressure from straining during a bowel movement, persistent diarrhea, or pregnancy. There are two types of hemorrhoids: internal and external.
Internal hemorrhoids are blood vessels on the inside of your anal opening. When they fall down into the anus as a result of straining, they become irritated and start to bleed. Ultimately, internal hemorrhoids can fall down enough to prolapse (sink or stick) out of the anus.
Treatment includes:
Improving bowel habits (such as avoiding constipation, not straining during bowel movements and moving your bowels when you have the urge).
Your healthcare provider using ligating bands to eliminate the vessels.
Your healthcare provider removing them surgically. Surgery is needed only for a small number of people with very large, painful and persistent hemorrhoids.
External hemorrhoids are veins that lie just under the skin on the outside of the anus. Sometimes, after straining, the external hemorrhoidal veins burst and a blood clots form under the skin. This very painful condition is called a “pile.”
Treatment includes removing the clot and vein under local anesthesia and/or removing the hemorrhoid itself.
Anal fissures
Anal fissures are also a structural disease. They are splits or cracks in the lining of your anus. The most common cause of an anal fissure is the passage of very hard or watery stools. The crack in the anal lining exposes the underlying muscles that control the passage of stool through the anus and out of the body. An anal fissure is one of the most painful problems your can have, because the exposed muscles become irritated from exposure to stool or air. This leads to intense burning pain, bleeding, or spasms after bowel movements.
Initial treatment for anal fissures includes pain medicine, dietary fiber to reduce the occurrence of large, bulky stools and sitz baths (sitting in a few inches of warm water). If these treatments don't relieve your pain, surgery might be needed to repair the fissure.
Perianal abscesses
Perianal abscesses, also a structural disease, can occur when the tiny anal glands that open on the inside of your anus become blocked, and the bacteria always present in these glands causes an infection. When pus develops, an abscess forms. Treatment includes draining the abscess, usually under local anesthesia in the healthcare provider’s office.
Anal fistula
An anal fistula – again, a structural disease – often follows drainage of an abscess. It's an abnormal, tube-like passageway from the anal canal to a hole in the skin near the opening of your anus. Body wastes traveling through your anal canal are diverted through this tiny channel and out through the skin, causing itching and irritation. Fistulas also cause drainage, pain and bleeding. They rarely heal by themselves and usually need surgery to drain the abscess and "close off" the fistula.
Diverticular disease
Diverticulosis is the presence of small outpouchings (diverticula) in the muscular wall of your large intestine that form in weakened areas of the bowel. They usually occur in the sigmoid colon, the high-pressure area of the lower large intestine. Diverticular disease is very common and occurs in 10% of people over age 40 and in 50% of people over age 60 in Western cultures. It is often caused by too little roughage (fiber) in the diet. Diverticulosis can sometimes develop/progress into diverticulitis
Complications of diverticular disease happen in about 10% of people with outpouchings. They include infection or inflammation in the pouches (diverticulitis), which can lead to bleeding and obstruction. Treatment of diverticulitis includes treating the constipation and sometimes antibiotics if really severe. Surgery is needed as last resort in those who have significant complications to remove the involved diseased segment of the colon.
Colon polyps and cancer
Fortunately, with advances in early detection and treatment, colorectal cancer is one of the most curable forms of the disease. By using a variety of screening tests, it is possible to prevent, detect and treat the disease long before symptoms appear.
THE IMPORTANCE OF COLORECTAL CANCER SCREENING
Almost all colorectal cancers begin as colon polyps, benign (non-cancerous) growths in the tissues lining your colon and rectum. Cancer develops when these polyps grow and abnormal cells develop and start to invade surrounding tissue. Removal of polyps can prevent the development of colorectal cancer. Almost all precancerous polyps can be removed painlessly during a colonoscopy screening. If not caught in the early stages, colorectal cancer can spread throughout the body. More advanced cancer requires more complicated surgical techniques.
Most early forms of colorectal cancer do not cause symptoms, which makes screening especially important. When symptoms do occur, the cancer might already be quite advanced. Symptoms include blood on or mixed in with the stool, a change in normal bowel habits, narrowing of the stool, abdominal pain, weight loss, or constant tiredness.
Most cases of colorectal cancer are detected in one of four ways:
By screening people at average risk for colorectal cancer beginning at age 45.
By screening people at higher risk for colorectal cancer (for example, those with a family history or a personal history of colon polyps or cancer).
By investigating the bowel in patients with symptoms.
A chance finding at a routine check-up.
Early detection is the best chance for a cure.
Colitis
There are several types of colitis, which are conditions that cause an inflammation of the bowel. These include:
Infectious colitis.
Ulcerative colitis (cause unknown).
Crohn's disease (cause unknown).
Ischemic colitis (caused by not enough blood going to the colon).
Radiation colitis (after radiotherapy).
Colitis can cause diarrhea, rectal bleeding, abdominal cramps and urgency (frequent and immediate need to empty the bowels). Treatment depends on the diagnosis, which is made by colonoscopy and biopsy.
There are many other gastrointestinal diseases. peptic ulcer disease, gastritis, gastroenteritis, celiac disease, Crohn's disease, gallstones, fecal incontinence, lactose intolerance, Hirschsprung disease, abdominal adhesions, Barrett's esophagus, appendicitis, indigestion (dyspepsia), intestinal pseudo-obstruction, pancreatitis, short bowel syndrome, Whipple’s disease, Zollinger-Ellison syndrome, malabsorption syndromes and hepatitis.
Many factors can upset your GI tract and its motility (ability to keep moving), including:
Eating a diet low in fiber.
Not getting enough exercise.
Traveling or other changes in routine.
Eating large amounts of dairy products.
Stress.
Resisting the urge to have a bowel movement, possibly because of hemorrhoids.
Overusing anti-diarrheal medications that, over time, weaken the bowel muscle movements called motility.
Taking antacid medicines containing calcium or aluminum.
Taking certain medicines (especially antidepressants, iron pills and strong pain medicines such as narcotics).
Pregnancy.
Some people also have heightened sensitivity in the organs of their GI tract (visceral hypersensitivity). This can make them feel pain or discomfort even when the organs are functioning normally.
Can gastrointestinal diseases be prevented?
Many intestinal disease can be prevented or minimized by maintaining a healthy lifestyle, practicing good bowel habits and getting screened for cancer.
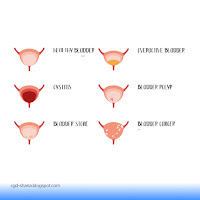
Urinary (Excretory) System
The urinary system is made up of the:
Kidneys
Ureters
Bladder
Urethra
These organs work together to filter blood and remove toxins and waste from body tissues. The removal of excess fluid through this organ system also helps regulate blood pressure.
What is the main function of the urinary system?
Urinary system filters blood to get rid of what body doesn’t need. It eliminates extra water and salt, toxins and other waste products. Different parts of the urinary system perform tasks, including:
Filtering blood.
Separating the toxins doesn’t need from the nutrients we do need.
Storing and carrying pee out of our body.
How does the urinary system filter blood?
Kidneys are an essential part of filtering blood. Here’s how the urinary system works:
Blood enters each kidney through lots of little arteries.
kidneys filter blood, separating toxins from nutrients.
Vitamins, minerals, nutrients and proteins return back to bloodstream.
Waste products and pee move from kidneys through ureters and bladder.
Bladder stores pee until we use the toilet.
Pee leaves our body through urethra.
What are the organs of the urinary system?
The kidneys, ureters, bladder and urethra make up the urinary system. They all work together to filter, store and remove liquid waste from body. All of the organs in urinary system are in our abdominal and pelvic region.
Here’s what each organ does:
Kidneys: These organs work constantly.
They filter blood and make pee, which our body then eliminates. We have two kidneys, one on either side of the back of our abdomen, just below our rib cage. Each kidney is about as big as fist. Our kidneys work hard — they filter about 120 to 150 quarts (113.6 to 141.95 liters) of blood per day, which produces about 1 to 2 quarts ( 0.95 to 1.95 liters) of pee each day.
Ureters: These two thin tubes inside our pelvis carry pee from kidneys to bladder. Each ureter is about 9 inches long.
Bladder: Bladder holds pee until we are ready to empty it (pee). It’s hollow, made of muscle, and shaped like a triangular balloon. Bladder expands as it fills up. Most bladders can hold up to 2 cups (500 milliliters) of pee at a time. Peeing is when we empty our bladder.
Urethra: This tube carries pee from bladder out of our body. We have two sphincter muscles that close off urethra to keep pee in when we aren’t using the toilet. These ring-like muscles open and close to let pee out. Sometimes, these muscles weaken and it becomes hard to hold our pee in.
CONDITIONS AND DISORDERS
What conditions and diseases affect the urinary system?

Many conditions can affect ureters, kidneys, bladder and urethra. Infections, diseases or problems can appear at birth or develop as get older. Cancer can also affect certain parts of urinary tract.
Some common urinary disorders are:
Infections
Urinary tract infections and sexually transmitted infections (STIs) can cause issues with kidneys, urethra or bladder. These infections occur when bacteria enter urinary tract through urethra.
Kidney stones
Kidney stones are small masses that form when waste products clump together. Kidney stones or ureteral stones (kidney stones that move to ureter) can cause severe pain and block the flow of pee.
Urination problems
Loss of bladder control or urinary incontinence (leakage), causes pee to leak when we don’t want it to. It can be worse when cough, laugh, sneeze or jump. Overactive bladder happens when feel the sudden urge to pee more often. Urinary retention is a condition where bladder doesn’t completely empty each time.
Many of these conditions consist of lower urinary tract symptoms like an urge to pee, a weak urine stream and leaking pee. Medications and lifestyle modifications can help treat these conditions.
Urinary tract obstructions
Growths or tumors in any part of urinary tract can affect the flow of pee. An enlarged prostate can block ureter so it’s harder to pee. Other causes of ureteral obstruction include pregnancy and gastrointestinal (GI) issues like Crohn’s disease. Bladder outlet obstruction can also happen and prevent bladder from emptying. Surgery can often help with obstructions in urinary tract.
Kidney disease
Kidney disease is a common and serious condition that affects urinary system. The most common causes of chronic kidney disease (CKD) are high blood pressure and diabetes. Managing blood pressure and blood sugar is crucial to lowering risk of kidney disease. Kidney disease can lead to kidney failure. Kidney failure may require dialysis or a kidney transplant.
Interstitial cystitis
Also called painful bladder syndrome, this condition causes inflammation in bladder. Medications and physical therapy can improve the symptoms of painful bladder syndrome.
Structural problems
Sometimes, babies are born with conditions that affect the way their urinary tract forms. For example, an ectopic ureter is when your child’s ureter connects to a place other than their bladder. Other urinary system organs can be underdeveloped, which can lead to issues with peeing.
A bladder prolapse is when bladder drops into vagina or hangs out of vaginal opening. Sometimes surgery is required to fix the problem.
How can I keep urinary system healthy?
You can try to keep your urinary system healthy with proper hygiene and a healthy lifestyle. To help your urinary system work the way it should, you can:
Drink plenty of water: Staying hydrated will flush out your system and can help you prevent kidney stones and UTIs.
Eat a balanced diet: Low-sodium, high-calcium foods may prevent kidney stones.
Empty your bladder fully: Make sure you let all of your pee out when you use the toilet. Don’t hold pee in for long periods of time.
Wipe/ clean with water the right way: If you have a vagina, you should always wipe / clean with water front to back after using the toilet. Proper wiping / cleaning reduces the risk of bacteria getting into your vagina and causing a UTI.
Empty your bladder after sex: If you have a vagina, you should use the bathroom after having sex. Peeing promptly can clear out bacteria and reduce your risk of a UTI.
Practice safe sex: Protect yourself from sexually transmitted infections with a condom.
Do pelvic floor exercises: Also called Kegel exercises, these can reduce your risk of urinary incontinence by strengthening the muscles in your pelvic floor.
Keep your genital area clean: Use water to clean your genitals and try to bathe or shower daily. Wear comfortable, loose underwear.
When should contact with doctor if I think I might have a problem with my urinary tract?
You should contact your healthcare provider if you’re having trouble or pain when you pee. It may be a sign of an infection or another condition.
Blood in your pee (hematuria).
Burning sensation, pain or difficulty peeing.
Pain in your pelvic area, lower back, genital area or flank (the back and sides of your abdomen).
Trouble holding your pee or problems with leaking pee.
A feeling that something is bulging out of your vagina.
Urinary system plays a critical role in keeping you alive. It filters your blood and removes waste and excess water through your pee. Your urinary system includes your kidneys, ureters, bladder and urethra. Conditions like urinary tract infections (UTIs), sexually transmitted infections (STIs), kidney diseases and urinary tract obstruction can affect the health of your urinary system. If you have one of these conditions, talk to your healthcare provider about steps you can take to stay healthy.
 |
| Use NO PAIN be relieved |
Reproductive system disease, any of the diseases and disorders that affect the human reproductive system. They include abnormal hormone production by the ovaries or the testes or by other endocrine glands, such as the pituitary, thyroid, or adrenals. Such diseases can also be caused by genetic or congenital abnormalities, infections, tumours, or disorders of unknown cause.
varicocele
The main divisions are concerned with
(1) genetic and congenital abnormalities,
(2) functional genital disorders,
(3) infections,
(4) structural changes of unknown cause, and
5) tumours. For discussion of diseases and disorders affecting pregnancy, see pregnancy. For diseases and disorders affecting childbirth, see parturition. Hormonal disorders affecting reproductive organs and functions are also discussed in the article human endocrine system.
Genetic and congenital abnormalities
In the male
Congenital anomalies of the prostate gland and seminal vesicles are rare; they consist of absence, hypoplasia (underdevelopment), or the presence of fluid- or semisolid-filled sacs, called cysts.
Cysts of the prostatic utricle (the uterine remnant found in the male) are often found in association with advanced stages of hypospadia and pseudohermaphroditism, a condition in which sex glands are present but bodily appearance is ambiguous as to sex; the secondary sexual characteristics are underdeveloped. Cysts may also cause urinary obstructive symptoms through local pressure on the bladder neck.
Severe anomalies of the penis are rare and are generally associated with urinary or other systemic defects that are incompatible with life.
Anomalies are those of absence, transposition, torsion (twisting), and duplication of the penis. An abnormally large penis frequently is present in males with precocious puberty, dwarfism, an overactive pituitary, or adrenal tumours. A small penis is seen in infantilism and in underdevelopment of the genitals, or undersecretion of the pituitary or pineal gland, and failure of development of the corpora cavernosa (erectile tissue located on the dorsal side of the penis).
The only anomaly of the foreskin is congenital phimosis, characterized by a contracture of the foreskin, or prepuce, which prevents its retraction over the glans (the conical structure that forms the head of the penis); the preputial opening may impede the flow of urine. The condition is treated by circumcision.
There is a considerable variety of urethral anomalies. Stenosis (contracture) of the external opening (meatus) is the most common, but congenital stricture of the urethra occasionally occurs at other points. Valves (or flaps) across the anterior or posterior part of the urethra may cause congenital urethral obstruction in males. Posterior urethral valves are more common than anterior valves and consist of deep folds of mucous membrane, often paper-thin and usually attached at one end to the verumontanum, a small prominence in the back wall of the part of the urethra that is surrounded by the prostate gland. If too tight, the valves may obstruct the urethra and damage the kidneys.
Various defects are associated with incomplete closure of the urethra. One of the most common is hypospadias, in which the underside (ventral side) of the urethral canal is open for a distance at its outer end. Frequently the meatus is narrowed, and the penis also has a downward curvature beyond the meatus. The posterior part of the urethra is never involved; therefore, the muscle that closes the urethra functions normally, and urinary control exists. Although the condition occurs in both sexes, it is seen predominantly in the male. There is a high incidence of partial or complete failure of the testes to develop, of cryptorchidism (failure of one or both of the testes to descend into the scrotum), and of small external and internal genitalia.
Epispadias, an opening in the upper (dorsal) side of the penis, is considerably less common than hypospadias. Dorsal curvature may also be present, but the disabling aspect is that the defect usually extends through the urinary sphincter and causes urinary incontinence. Other less common urethral anomalies include complete absence of the urethra, double urethra, urethra fistula (an opening in the urethra), urethrorectal fistula (an opening between the urethra and the rectum), and urethral diverticulum (a pouch in the wall of the urethra). Most of the above conditions are correctable by surgery.
Anorchism (absence of one or both testes) is rare; it may be associated with the absence of various other structures of the spermatic tract. Generally, if one testis (also called testicle) is absent, the other is found to be within the abdomen rather than in the scrotum. Congenitally small testes may be a primary disorder or may occur because of underactivity of the pituitary. In both disorders, there is a lack of development of secondary sexual characteristics and some deficiency in libido and potency. Supernumerary testicles are extremely rare; when present, one or more of the supernumerary testicles usually shows some disorder such as torsion of the spermatic cord. Synorchism, the fusion of the two testicles into one mass, may occur within the scrotum or in the abdomen. Cryptorchidism, the most common anomaly of the spermatic tract, is the failure of one or both of the testes to descend spontaneously into the scrotum; hormonal treatment may be useful in correcting the condition, but usually surgery is necessary for correction.
In the female
The female external genitalia are less complex than those of the male but have anomalies that can at times severely interfere with the functioning of the female urogenital tract.
What is the female reproductive system’s function?
From birth, a girl has all the eggs she will have throughout her life, although these cannot become babies until puberty begins, at which time the hormones released in the body will cause the ovaries’ development.
Once the ovaries begin to develop, they will generate estrogen which will result in the development of the entire female reproductive system.
What common diseases occur in the female reproductive system?
Female reproductive system diseases are considered to be all those that occur in the vagina, cervix and uterus, breasts, or ovaries.
This type of diseases can have different origins, ranging from poor hygiene, the existence of fungi, or even genetic or hereditary factors. Although female reproductive system diseases can arise at any stage of life, it is very common that, after the age of 40, the moment in which they go through menopause, they appear more frequently.
Among the common female reproductive system diseases are:
Cervical Cancer. Also known as uterine cancer, it occurs most often in women who are obese or during the first stage of menopause.
Breast cancer. It originates in breast tissue and there are different types depending on its origin.
Vaginal yeast infection. It is one of the most common diseases and is caused by a fungus that arises due to the alteration of the pH of the vaginal discharge or a weak immune system.
Endometriosis. In the presence of tissue similar to the endometrium, it causes chronic inflammation and irregular menstruation.
STD. Although sexually transmitted diseases affect both men and women, in many cases in women they can cause more serious symptoms or complications.
Urinary infections. Due to the presence of bacteria in the urethra, this infection can result in cystitis or pyelonephritis.
Uterine prolapse. Alteration of the pelvic ligaments that results in the lack of adequate support in the uterus.
Ovarian cyst. Although some cysts may disappear on their own, they can cause complications if they don’t.
HPV. The human papillomavirus is one of the most common pathologies and can cause warts on the sexual organs or promote the development of cancer.
 |
| Use LD DETOXIFICATIOON |
There are ways to keep your reproductive system healthy. What can you do to keep your reproductive system healthy? You can start by making the right choices for overall good health. To be as healthy as you can be, you should:
Eat a balanced diet that is high in fiber and low in fat.
Drink plenty of water.
Get regular exercise.
Maintain a healthy weight.
Get enough sleep.
Avoid using tobacco, alcohol, or other drugs.
Manage stress in healthy ways.
Disorders of the Immune System
Your immune system is your body’s defense against infections and other harmful invaders. Without it, you would constantly get sick from bacteria or viruses.
Your immune system is made up of special cells, tissues, and organs that work together to protect you.
What can go wrong with your immune system?
When your immune system doesn't work the way it should, it is called an immune system disorder. You may:
Be born with a weak immune system. This is called primary immune deficiency.
Immune system disorders
Severe combined immunodeficiency (SCID). This is an example of an immune deficiency that is present at birth. Children are in constant danger of infections from bacteria, viruses, and fungi. This disorder is sometimes called “bubble boy disease.” In the 1970s, a boy had to live in a sterile environment inside a plastic bubble. Children with SCID are missing important white blood cells.
Temporary acquired immune deficiencies. Your immune system can be weakened by certain medicines, for example. This can happen to people on chemotherapy or other drugs used to treat cancer. It can also happen to people following organ transplants who take medicine to prevent organ rejection. Also, infections like the flu virus, mono (mononucleosis), and measles can weaken the immune system for a brief time. Your immune system can also be weakened by smoking, alcohol, and poor nutrition.
AIDS. HIV, which causes AIDS, is an acquired viral infection that destroys important white blood cells and weakens the immune system. People with HIV/AIDS become seriously ill with infections that most people can fight off. These infections are called “opportunistic infections” because they take advantage of weak immune systems.
An overactive immune system
If you are born with certain genes, your immune system may react to substances in the environment that are normally harmless. These substances are called allergens. Having an allergic reaction is the most common example of an overactive immune system. Dust, mold, pollen, and foods are examples of allergens.
Some conditions caused by an overactive immune system are:
In autoimmune diseases, the body attacks normal, healthy tissues. The cause is unknown. It is probably a combination of a person’s genes and something in the environment that triggers those genes.
Three common autoimmune diseases are:
Rheumatoid arthritis. This type of arthritis causes swelling and deformities of the joints. An auto-antibody called rheumatoid factor is in the blood of some people with rheumatoid arthritis.
Lupus. This disease that attacks body tissues, including the lungs, kidneys, and skin. Many types of auto-antibodies are found in the blood of people with lupus.
Healthy ways to strengthen your immune system
Don't smoke.
Eat a diet high in fruits and vegetables.
Exercise regularly.
Maintain a healthy weight.
If you drink alcohol, drink only in moderation.
Get adequate sleep.
Take steps to avoid infection, such as washing your hands frequently and cooking meats thoroughly.
Try to minimize stress.
Keep current with all recommended vaccines. Vaccines prime your immune system to fight off infections before they take hold in your body.
































































Comments