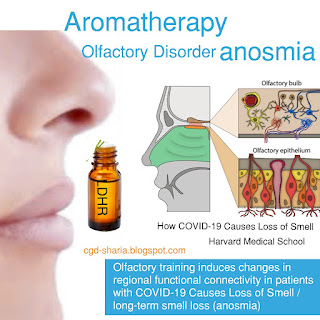
Olfactory Disorder ANOSMIA ( total loss of smell) and Aromatherapy(smell training)
Some common definition :
- Anosmia - tatal loss of smell.
- Ageusia - loss of taste function of the tongue.
- Specific anosmia - the inability to detect particular smell or smells.
- Hyposmia - reduced olfactory function.
- Dysosmia - a qualitative change of the sense of smell.
- Hyperosmia - increased ability to smell odours to abnormal levels. This is very rare and often associated with migraines.
- Parosmia - a different sense of smell, that is a smell is perceived as another usually a very unpleasant smell.
- Phontosmia - perceiving a smell that is not actually there.
The most common reported causes of smell losses are -
- Post-viral upper respiratory tract infections (18 to 45℅ of the clinical population)
- Nasal or sinus diseases( 7 to 56%)
- Head traumas ( 8 to 20℅)
- Exposure to toxins and drugs (2 to 65%)
- Congenital loss (0 to 4℅)
A study from Virginia Commonwealth University reported the sense of smell or taste returns within six months for 4 out of every 5 COVID-19 patients who have lost these senses, and those under 40 are more likely to recover these senses compared to older patients.
This paper went on to report that using smell training using essential oils may help.
A report from the University of East Anglia also suggested that smell training could be beneficial. This involves sniffing at least four different odours twice a day every day for several months. Smell training is reported as an inexpensive, simple and side-effect free treatment option for various causes of smell loss, including COVID-19.
The aim of smell training is to help
- recovery based on neuroplasticity;
- allowing the brain to reorganise itself to compensate for a change or injury.
Pathophysiology of SARS-CoV-2 infection on olfaction
- Inflammatory damage
- Infection of olfactory epithelium
- Relationship between anosmia and covid-19 fatigue syndrome
- Covid19 and the brain
- The genetic link
SARS-CoV-2 infects host cells by the virus’s spike protein binding to the viral receptors angiotensin-converting enzyme 2 (ACE2) and transmembrane serine protease 2 (TMPRSS2). Both of these receptors are highly expressed in the gastrointestinal tract, in the nasal and bronchial epithelium as well as in the type II alveolar epithelial cells.
The data from research indicates that COVID-19 related anosmia may arise from temporary loss of function of the supporting cells in the olfactory epithelium, which results in the impairment of olfaction. The researchers do not fully understand why olfactory impairment occurs.
It is also suggested that COVID-19 anosmia occurs with the increase in the levels of interleukin-6 (IL-6), an important pro-inflammatory cytokine which leads to inflammatory damage to the olfactory epithelium. It is suggested that an inflammatory cytokine environment in the nasal cavity would also potentially affect olfactory neuronal function, as in rhinosinusitis.
Therapies for smell disordersi:
Phenyl ethyl alcohol (from rose), eucalyptol (from eucalyptus or rosemary), citronella and eugenol (from clove bud) are four of the six odours that have been used to improve olfactory loss after training for 12 weeks or more.
Salvatore Battaglia, my suggestion is to use a rich floral such as ylang ylang or rose, a spicy aroma such as clove bud, a eucalyptol-rich oil such as rosemary or eucalyptus, and a rich lemon-scented oil such as lemon, lemon myrtle or citronella.
While the efficacy of olfactory training is disputed, a systematic review supports the use of olfactory training for all patients with a loss of smell.
It is also noted that the Rhinology Societpy recommend olfactory training for patients who complain of hyposmia or anosmia for more than 2 weeks.
It is highly recommended that smell training be considered as a treatment. Smell training has no known side effects and is low cost.
Other options investigated for olfactory dysfunction included:
- Zinc
- Vitamin A
- Alpha-lipoic acid (ALA)
- Omega 3 fatty acids
- Use of corticosteroids
Coronavirus
References
- https://www.salvatorebattaglia.com.au/blog/137-covid-19-and-anosmia
- 1. Huart C et al. Systemic corticosteroids in coronavirus disease 2019 (COVID-19)-related smell dysfunction: an international view. International Forum of Allergy & Rhinology. 2021;11(7):1041-1046. doi:10.1002/air.22788
- 2. University of East Anglia, Smell training, not steroids, best treatment for COVID-19 smell loss, research finds. Apr 26, 2021, downloaded on 3 Nov 20221 from https://www.sciencedaily.com/releases/2021/04/210426140845.htm
- 3. Renaud M et al. Clinical outcomes for patients with anosmia 1 year after COVID-19 diagnosis. JAMA Network Open. 2021;4(6):e2115352. doi:10.1001/jamanetworkopen.2021.15352
- 4. Virginia Commonwealth University, Those under 40 are more likely than older adults to recover COVID-related smell and taste loss, study finds. Oct 5, Sep 2021, downloaded on 3 Nov 2021 from https://www.sciencedaily.com/releases/2021/10/211005124655.htm
- 5. Neta FI et al. Pathophysiology and possible treatments for olfactory-gustatory disorders in patients affected by COVID-19. Current Research in Pharmacology and Drug Discovery. 2021: 1000035. doi:10.1016/j.crpar.2021.100035
- 6. Jiang K, How COVID-19 causes loss of smell. Downloaded on 3 Nov 2021 from https://hms.harvard.edu/news/how-covid-19-causes-loss-smell
- 7. Brann DH et al. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Science Advances. 2020:6:eabc5801, 31 July 2020.
- 8. Burges Watson DL. Et al. Altered smell and taste: anosmia, parosmia and the impact of long Covid-19. PLoS ONE 2021;16(9):e0256998. doi:10.1371/journal.pone.0256998
- 9. University of York, Nov 5, 2018. Is there a universal hierarchy of human senses? Downloaded on 4 Nov 2021 from https://www.sciencedaily.com/releases/2018/11/181105160852.htm
- 10. University of Cincinnati, Research examines coping mechanisms for loss of smell from COVID-19. Oct 25, 2021, downloaded on 3 Nov 2021 from https://www.sciencedaily.com/releases/2021/10/211025113738.htm
- 11. Hummel T et al. Position paper on olfactory dysfunction. Rhinology – Official Journal of the European and International Societies. 2017;54(Supplement 26).
- 12. Hopkins C et al. Management of new onset loss of sense of smell during the COVID-19 pandemic – BRS concensus guidelines. Clinical Otolaryngology. 2021;46:16-22. Doi:10.1111/coa.13636
- 13. Singh CV et al. The outcome of fluticasone nasal spray on anosmia and triamcinolone oral paste in dysgeusia in COVID-19 patients. American Journal of Otolaryngology. 2021;42(3):102892. doi:10.1016/j.amjoto.2020.102892





















Comments